- cross-posted to:
- cfs@lemmit.online
- cross-posted to:
- cfs@lemmit.online
Background
A considerable number of patients who contracted SARS-CoV-2 are affected by persistent multi-systemic symptoms, referred to as Post-COVID Condition (PCC). Post-exertional malaise (PEM) has been recognized as one of the most frequent manifestations of PCC and is a diagnostic criterion of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Yet, its underlying pathomechanisms remain poorly elucidated.
Results
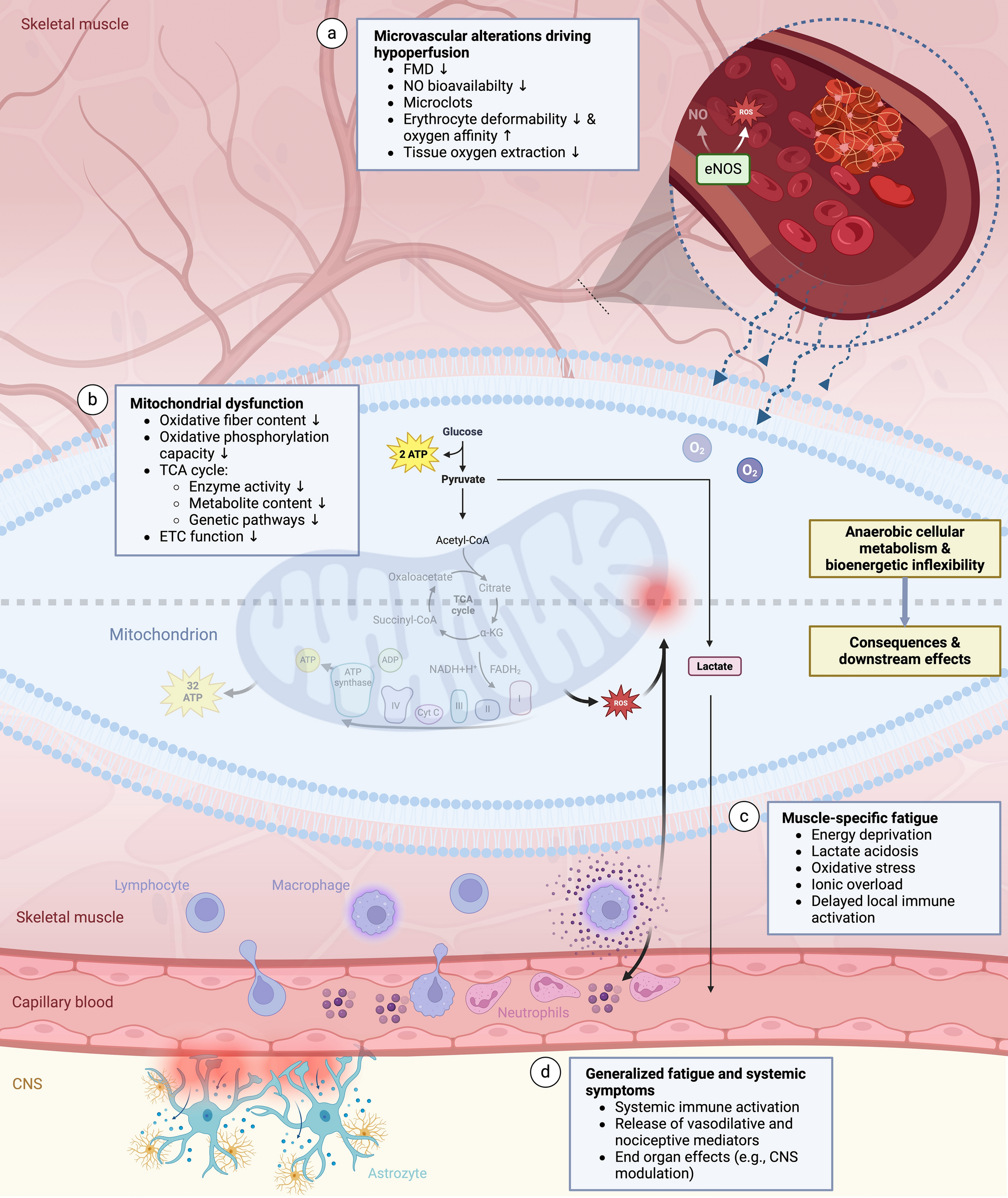
Upon physical activity, affected patients exhibit a reduced systemic oxygen extraction and oxidative phosphorylation capacity. Accumulating evidence suggests that these are mediated by dysfunctions in mitochondrial capacities and microcirculation that are maintained by latent immune activation, conjointly impairing peripheral bioenergetics. Aggravating deficits in tissue perfusion and oxygen utilization during activities cause exertional intolerance that are frequently accompanied by tachycardia, dyspnea, early cessation of activity and elicit downstream metabolic effects. The accumulation of molecules such as lactate, reactive oxygen species or prostaglandins might trigger local and systemic immune activation. Subsequent intensification of bioenergetic inflexibilities, muscular ionic disturbances and modulation of central nervous system functions can lead to an exacerbation of existing pathologies and symptoms

There’s a feature of some Long COVID cases (~50%) which is also the defining feature of an illness called ME/CFS which has been caused by various forms of viral infections throughout history. (It is thought that a lot of Long COVID cases are ME/CFS). Anyways this feature is, Post-Exertional Malaise, a worsening of the illness after exertion beyond a certain threshold, which can entail hundreds of symptoms and be permanent.
This paper is a review of some of the biomedical studies looking at what could possibly cause this, and finds there is repeated data of Microvascular (blood vessels) and immunometabolic (metabolic markers relating to immune function) differences with healthy controls.
The leading hypotheses are that this is caused by mitochondrial dysfunction which is mediated by a dysregulated immune system.
Some of my colleagues were co-authors on this paper. I’ll forward the feedback that it is jargony.
Thank you.
Science communication is hard. If the audience is scientists in the field, the text is probably digestible, but for anyone else, it’s just not.
Note that I’m not saying anything about the content itself, but in my experience, considering who is reading is useful in most cases.